The City of Keene rescinded its mask mandate last week. I don’t know which data they might have looked at, but there is still a lot of virus around in the air. In my small grocery store example I presented in the Feb. 11th posting, where the odds were 99% to have one or more covid-positive people there in the store when I’m there, now it’s down to 96%!
Hooray, let’s celebrate and rip off those masks!
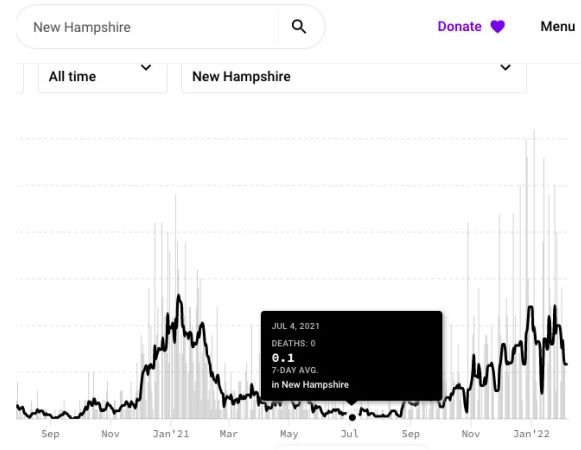
Below is a chart with some historical context, showing the two Keene mask mandates. Of course I would have waited for a hospitalization rate down to that of last July, or the grocery store odds down to 10%. If the next variant doesn’t get here too soon, I am hopeful that we might see similar low levels this coming summer.
Highlights From Past Blogs
February 16 - Ventilation Revolution
February 11 - When Will it Be "Safe?"
February 2 - Covid-19 Testing
January 27 - How Long Does Immunity Last?
January 20 - You Need a Fresh Air Meter
January 11 - Air Purifiers
January 4 - Masks That Actually Work
December 22 - Blog Intro and History
December 15 - The Double Risk of Indoor Dining
December 13 - Omicron Symptoms
December 10 - Simple Air Filtration
December 9 - Comprehensive Guide to Covid-19 Safety in Buildings
December 6 - Solution to Pollution is Dilution
November 24 - No Magic to Six Feet