As we have been advocating in this blog, the “new normal” does not have to be returning to the identical life as before the pandemic, since that translates into "let-the-virus-do-what-it-wants”, which is: continuing to put 40,000 Americans into hospitals and 400 into their graves EVERY DAY. This is a rate of about 150,000 deaths a year, THREE TIMES HIGHER than the WORST flu seasons of the last decade.
Covid-19 Deaths and Hospitalizations (Washington Post, Aug. 16, 2022):
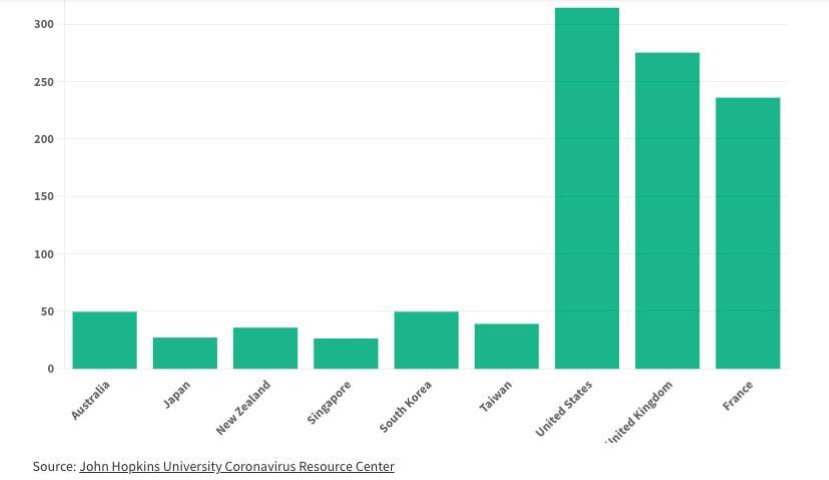
In the article linked below, a Vassar professor points out that several Asia-Pacific countries are setting an example of an intelligent new normal, with striking results compared to the U.S. For example, covid-19 mortality rates per 100,000 people:
How are they doing this? Simple stuff, which all adds up:
1 - higher vaccination rates
2 - ubiquitous indoor masking in the most important places
3 - widespread improved fresh air ventilation and air purification - - the subject of many entries in this blog, and which includes being aware of the quality of the fresh air by measuring it
I can suggest another item:
4 - effective use of antigen testing to ensure those gathering together are not contagious (see the previous blog post)
Here is the full article:
https://thediplomat.com/2022/08/how-third-way-countries-live-with-covid-19/
[The information contained in this article is for educational and informational purposes only and is not intended as health or medical advice. Always consult a physician or other qualified health provider regarding any questions you may have about a medical condition or health objectives.]
Now You Can Search This Blog!
We have added a “search” bar for this blog - scroll all the way down
to the very bottom of a blog page to find the search bar.
We invite you to subscribe to our Newsletter -
the cost is free and each new post comes to your email
every two weeks on Thursdays!
To subscribe, simply email safetulator@kohlerandlewis.com
with your name and email address and we will sign you up.
Highlights From Past Blogs
June 30 - Summer Gatherings Can Be Safer
June 22 - Summer Gatherings Can Be Safer
May 31 - Covid Myth-Busting
April 29 - The Big Meter
April 19 - The Spring Surge Is Here
April 7 - How to Test
March 21 - The Origin of the CDC’s Biggest Mistake
February 25 - One. Million. Deaths.
February 16 - Ventilation Revolution
January 11 - Air Purifiers
January 4 - Masks That Actually Work
December 15 - The Double Risk of Indoor Dining